
As many of you will know, my 86 year old mother had a bad fall last September in her bedroom in the middle of the night, triggering 4 months of pain, a myriad doctor’s appointments, increased carer hours and a mind boggling amount of medication.
Six weeks after her fall I wrote my first post about dealing with this, specifically dealing with the unknown, guessing at the trajectory that she might take, and worrying that this might be the start of a longer-term decline.
I am pleased to say that she is now fully recovered and in the best health I’ve seen her for some time. But the journey to get there has been challenging, including a battle for an Xray, an aborted respite stay in a care home and discovering the less-than-pleasant side effects of morphine.
So I thought it about time that I wrote a post about my experience, to share what I’ve learnt. Those of you reading this who have parents that you care for, either now or in the future, will very likely have to deal with a fall at some point. The more prepared, the better.
Just a note: my mother didn’t have a major break or have to be admitted to hospital, so this post doesn’t touch on that whole experience - a different ball game all together….
So, let’s start with morphine.

My mother has little experience of this strong painkiller except for 40 years ago when she was put on sky high doses after suffering life-threatening injuries in our family car accident. She remembers little apart from the colourful hallucinations they triggered (she was convinced she was in a hospital bed in Hong Kong – a place she’s never been to - and could describe the sky scrapers outside her window!)
A couple of weeks after her fall, the doctor prescribed morphine tablets as the codeine wasn’t effective. He was reluctant to do this as he knows the side effects. But we didn’t. After a week she started to experience confusion and she became more unsteady on her feet. After a month her stomach became unsettled and she lost her appetite. After two months rashes appeared on her skin. It was not quite debilitating.
Becoming more unsteady on her feet was a real concern, for obvious reasons. And the confusion was distressing for her: she wasn’t able to manage her emails or finances, got totally muddled with passwords, ordering her online shop and even remembering the time of day. One time she asked for soup for her breakfast, thinking it was lunchtime as she’d been awake for so long. Even more alarmingly, when she was on the highest dose, she started to have that same hallucination about being in Hong Kong! The mind is a curious thing.
Between myself and the carer we managed to keep her safe, but the fact that she knew she was making mistakes made it all the more difficult and distressing for her.
So, if your parent is put on morphine, be prepared. Ensure they have good care, be in regular contact with the carer (where you can) aswell as their GP. With GP services so over-stretched, the onus is often on the patient to let the GP know how they are responding to the medication but they are often not ‘with it’ enough to email her GP regularly enough with how the medication was affecting her.
And ask your parent to email their GP to give you the authority to speak on their behalf. Doing this before they fall can make all the difference.
Next up, that X-ray.
As I wrote in my first post, the GP thought the pain was caused by muscle spasm in her buttocks and lower back. Her private physio (who she sees about another issue) agreed. The GP did not refer her for an Xray as he said that if even it showed a fracture, the treatment would be the same – pain relief drugs and rest.
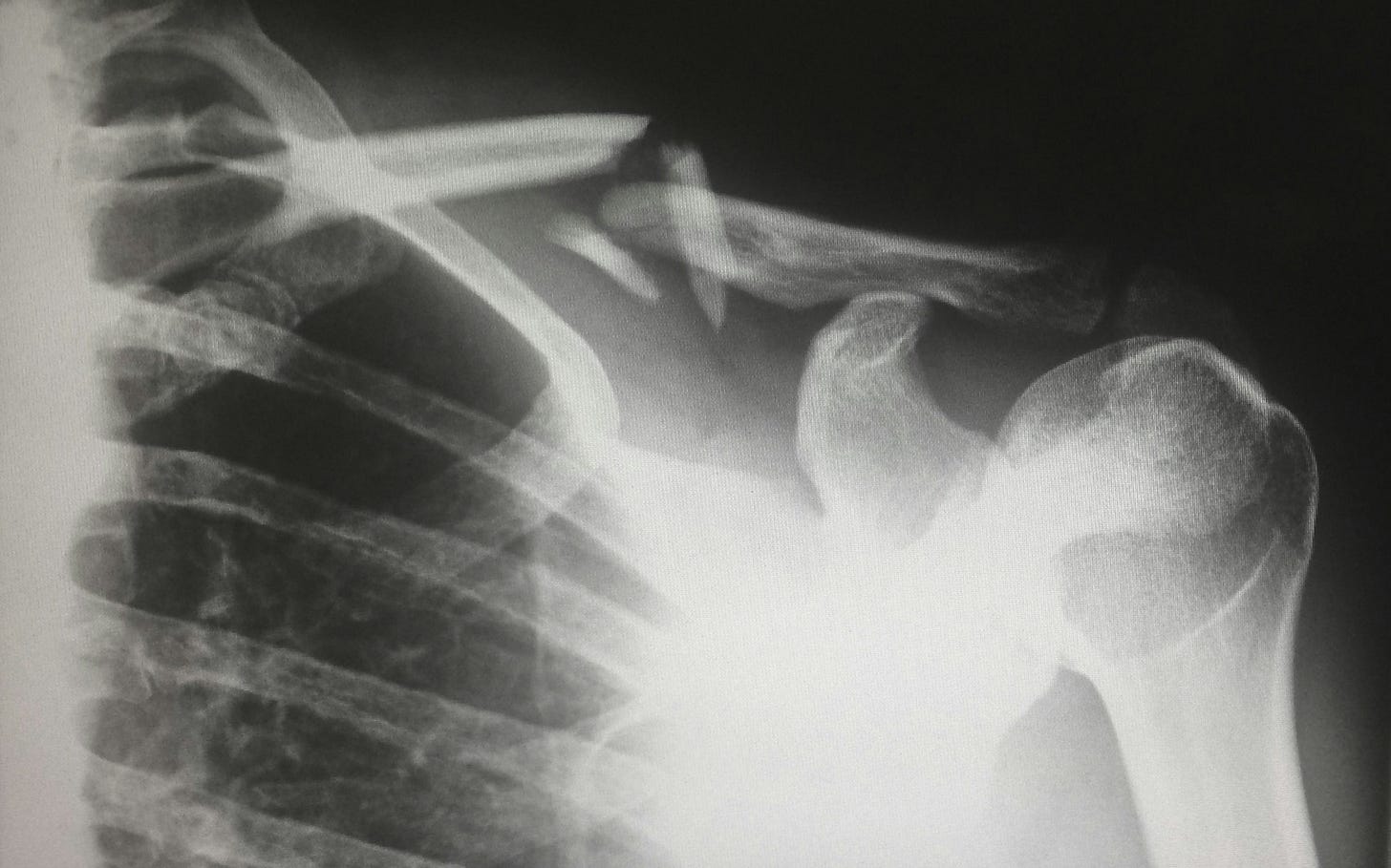
However, it was only after the NHS physio from the Falls team (from our local NHS trust) came to assess her that we realised the importance of an Xray. The physio said he could not advise on the correct treatment plan without being sure of the injury. This was one month after the fall. It took another 3 weeks for her to get an appointment at our local hospital for the Xray and another week to get the result, totalling 8 weeks after her fall.
The Xray found she did, in fact, have a compression fracture. Although this diagnosis didn’t change the medication, as the GP had said, it did give her peace of mind knowing what the injury was. We are puzzled why he didn’t refer her earlier, in the light of what the physio had said. He is an excellent GP from a very good surgery. That said, it doesn’t seem to be uncommon. A couple of other people I’ve spoken to have said their GP also refused an Xray for their elderly parent after a fall who continued to have problems long term.
My advice to anyone in this situation is to ask your parent to discuss this properly with their GP - to explore whether a lack of clear evidence of the injury will affect their physio plan.
And lastly, that aborted respite visit to a care home….
I was due to go away for a week mid-October and although we had a carer coming in for an hour in the morning and evening, I felt Mum would benefit from a week’s rest in a care home. She could switch off from worrying about food shopping and I’d know she’d be looked out for 24/7. I also thought that a stay in a local care home would give her a feel for one should she need one in the future. So I investigated a few homes that had good reputations.
The one we landed on was recommended by the GP who did visits there. It had a general good reputation although we didn’t know anyone who’d been there recently. It was a pleasant looking home with apparently efficient staff, was well decorated and not over-heated (those homes where you come out gasping for air are simply dreadful!).
It was a bit of a disaster.
Although the staff were very pleasant and helpful, they were simply overrun and uninformed of my mother’s needs (e.g her poor mobility and regular need for changes of ice packs for pain relief). Resources were clearly stretched and communication systems weren’t working. As a result she had to keep buzzing for help throughout the day, even just getting water, and at night she had to hobble into the corridor to find someone to help her get ready for bed.
It was clear she had been shoe-horned in.
Not surprisingly, she hated it. After 48hrs she called me in tears asking me to bring her home. I realised we needed to abort. Whilst I realised it takes time for staff to get to know her, she didn’t have that time - especially when you’re paying £1,500 a week! The manager, clearly aware of the shortcomings, fully accepted our complaints and agreed to my mum leaving, albeit without refunding the amount for her 2 days stay.
Considering this was a care home that was part of a large chain, with a supposed good reputation, I was both alarmed and annoyed. The amount charged by these places is eye watering. Surely they can hire enough staff and equip them well enough to ensure they are able to do their jobs?
I learnt a few things from this debacle. Firstly, despite what websites and staff say, respite is, in the main, respite for carers, not so much for the person going in. So, if your parent has more than average needs, like Mum had, I wouldn’t advise putting them in respite - unless you have a good, recent and reliable recommendation. And this is my second learning. Be careful to get, if you can, recent recommendations. The standard of care in these homes can change very quickly given the fairly high turnover of operational managing staff. Lastly, a GP’s impression of a care home isn’t to be fully relied upon, at least not for respite. You can’t really judge a home without being on the receiving end of care.
Despite these challenges, my Mum has been grateful for the care she has received from her doctor’s surgery, paying her home visits where necessary. She also is aware of how lucky she’s been with the small care agency we use who have shown great care and flexibility. We couldn’t have got such flexibility from a bigger agency who usually need at least 2 weeks notice for a change.
And this was another lesson - having a care agency in place before my Mum had started to fall made all the difference. I mentioned the importance of getting care in place before it is fully needed in this post. If your parent can afford it, getting someone in for even just a few hours a week means you will be ready should they suddenly deteriorate and need more care. And if they can’t afford it, there’s always the non-means tested Attendance Allowance that they can claim for if they have a medical need (as mentioned in the above post).
I’ve had to learn some hard lessons from this experience, but at least I can share them with you! Of course, things will vary from county to county, and from country to country, but being aware of these issues and being prepared can make such a difference to you and your parent.
If you enjoyed reading this please tap the heart to like it, share it or subscribe for my fortnightly posts on living a Sandwiched Life.
I don’t yet charge, but if you’d like to give me a small tip, or even pledge your support to my publication, I’d be chuffed!
PS. The sun has actually come out for the first time in a fortnight here in Hertfordshire. Hope it has for you! Off to do a little jig…..





Sobering stuff. Thank you for sharing in such a balanced and measured way. God bless you. R x
Thanks for sharing this sound advice, Siobhan. I'm so glad that your mum is now doing well. I was intrigued by your parting comment... Do you dance? And, if so, what kind of dancing? I reckon there's nothing like it to lift the spirits! xx